Description
Uses and Administration of Erythropoietin in Kenya
Erythropoietin is a glycosylated protein hormone and a haematopoietic growth factor. It is secreted primarily by the kidneys, although a small amount is produced in extrarenal sites such as the liver. Erythropoietin regulates erythropoiesis by stimulating the differentiation and proliferation of erythroid precursors, stimulating the release of reticulocytes into the circulation, and stimulating the synthesis of cellular haemoglobin. The release of erythropoietin is promoted by hypoxia or anaemia, and up to 1000 times the normal serum-erythropoietin concentration may be reached under these conditions; this response may be impaired in some disease states such as chronic renal failure. The haematological response to erythropoietin is reduced if there is an inadequate supply of iron.
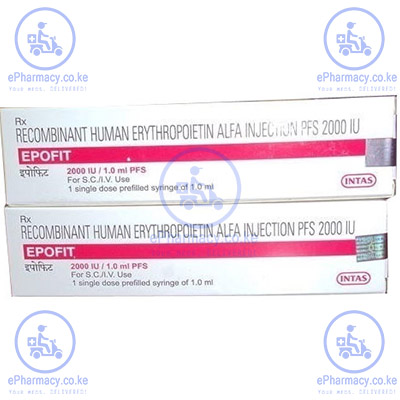
Epoetin alfa and epoetin beta are recombinant human erythropoietins available for clinical use in Kenya mostly marketed as; Recormon, Epofit and Relipoiten, that have the same pharmacological actions as endogenous erythropoietin. Recormon/Epofit/Relipoetin are used in the management of anaemia in Kenya associated with chronic renal failure in dialysis and predialysis patients; they may reduce or obviate the need for blood transfusions in these patients. They are also used in the management of chemotherapy-induced anaemia in patients with non-myeloid malignant disease. Epoetin alfa is used in zidovudine-related anaemia in HIV-positive patients. Epoetin beta is used in the management of anaemia of prematurity. Recombinant human erythropoietin is also being evaluated in the management of other types of normocytic-normochromic anaemias, including that associated with inflammatory disorders such as rheumatoid arthritis. In all patients in Kenya, iron status should be monitored and supplementation provided if necessary.
Epoetin alfa and epoetin beta may also be used in patients with moderate anaemia (but no iron deficiency) before elective surgery to increase the yield of blood collected for autologous blood transfusion. Epoetin alfa may also be used in such patients to reduce the need for allogeneic blood transfusion.
In the management of anaemia of chronic renal failure epoetin alfa or epoetin beta may be given subcutaneously or intravenously, depending on the formulation. The aim of treatment is to increase the haemoglobin concentration to 10 to 12 g per 100 mL or to increase the haematocrit to 30 to 36%. The rate of rise in haemoglobin should be gradual to minimise side-effects such as hypertension; a rate not exceeding 2 g per 100 mL per month is suggested.
Epoetin alfa may be given by intravenous injection over at least 1 minute; slow intravenous injection over 5 minutes may be used in patients who experience flu-like symptoms as side-effects. Epoetin alfa may also be given subcutaneously, but preparations that contain polysorbate 80 should only be given intravenously in this group of patients. In predialysis and haemodialysis patients, a recommended initial dose of epoetin alfa is 50 international units/kg three times weekly; a higher initial dose of 50 to 100 units/kg three times weekly has been suggested in the USA, hence applied in Kenya. Doses may be increased at 4-week intervals in increments of 25 units/kg three times weekly until the target is reached. In patients on peritoneal dialysis an initial dose of 50 units/kg given intravenously twice weekly may be used. Once the target is reached doses may need to be adjusted, and even decreased, for maintenance therapy.
The usual total weekly maintenance dose of epoetin alfa in predialysis patients is 50 to 100 units/kg given in three divided doses, and in haemodialysis patients it is about 75 to 300 units/kg given in three divided doses. In predialysis patients a total weekly dose of 600 units/kg should not be exceeded. In patients on peritoneal dialysis, the usual total weekly maintenance dose is 50 to 100 units/kg given intravenously in two divided doses.
In children, epoetin alfa may be given intravenously to those on haemodialysis at an initial dose of 50 units/kg three times weekly. The dose may be increased at 4-week intervals in increments of 25 units/kg three times weekly until a target haemoglobin concentration of 9.5 to 11 g per 100 mL is reached; the usual total weekly maintenance dose given in three divided doses is: 225 to 450 units/kg for those weighing less than 10 kg; 180 to 450 units/kg for those weighing 10 to 30 kg; and 90 to 300 units/kg for those weighing over 30 kg.
Epoetin beta is used similarly in the management of anaemia of chronic renal failure in dialysis and predialysis patients. It may be given subcutaneously or by intravenous injection over 2 minutes. The following dosages may be used in adults and children. For subcutaneous injection the initial dose is 60 units/kg weekly for 4 weeks; the total weekly dose may be divided to be given in daily doses or three times a week. For intravenous injection the initial dose is 40 units/kg three times weekly for 4 weeks; the dose may then be increased to 80 units/kg three times weekly. Thereafter the dose of epoetin beta may be increased at 4-week intervals, for both subcutaneous and intravenous injection, in increments of 60 units/kg weekly in divided doses, until the target haemoglobin concentration or haematocrit is reached. A total weekly dose of 720 units/kg of epoetin beta should not be exceeded. For maintenance, the dose is halved initially and then adjusted every 1 to 2 weeks according to response. The weekly subcutaneous maintenance dose may be divided into 1, 3, or 7 doses; in patients stabilised on a once-weekly administration, it may be possible to adjust to a single dose every 2 weeks.
In patients with non-myeloid malignant disease receiving chemotherapy, epoetin alfa or epoetin beta may be given by subcutaneous injection in an initial dose of 150 units/kg three times weekly. The dose may be increased after 4 or 8 weeks, if necessary, to 300 units/kg three times weekly. If the response is still inadequate after 4 weeks at this higher dose, treatment should be discontinued. As alternative regimens, the total weekly dose of epoetin beta may be given as a single dose or divided into 3 to 7 doses. The rate of rise in haemoglobin should be gradual; a rate not exceeding 2 g per 100 mL per month is suggested. After the end of chemotherapy, epoetin alfa or epoetin beta may be continued for up to one month.
To increase the yield of autologous blood, epoetin alfa or epoetin beta may be used with iron supplementation. The dose depends on the volume of blood required for collection and on factors such as the patient’s whole blood volume and haematocrit. Suggested regimens are: epoetin alfa 600 units/kg given intravenously twice weekly starting 3 weeks before surgery; or up to 800 units/kg of epoetin beta intravenously, or up to 600 units/kg subcutaneously, twice weekly for 4 weeks before surgery. To reduce the need for allogeneic blood transfusion epoetin alfa may be given in a dose of 600 units/kg subcutaneously once weekly starting 3 weeks before surgery, with a fourth dose given on the day of surgery; alternatively, when the time before surgery is short, 300 units/kg subcutaneously daily may be given for 10 days before surgery, on the day of surgery, and for 4 days after.
In HIV-positive patients on zidovudine therapy, epoetin alfa may be beneficial if the endogenous serum-erythropoietin concentration is 500 milliunits/mL or less. Epoetin alfa is given by subcutaneous or intravenous injection in an initial dose of 100 units/kg three times weekly for 8 weeks. The dose may then be increased every 4 to 8 weeks by 50 to 100 units/kg three times weekly according to response. However, Kenyan patients are unlikely to benefit from doses above 300 units/kg three times weekly if this dose has failed to elicit a satisfactory response.
In the management of anaemia of prematurity in Kenya, epoetin beta is given subcutaneously in a dose of 250 units/kg three times weekly. Treatment should be started as early as possible and continued for 6 weeks.
Adverse Effects and side effects of Recormon/Epofit in Kenya
Headache, hypertension, and seizures have been reported in some patients treated with recombinant human erythropoietin particularly in those with poor renal function. These adverse effects are probably associated with haemodynamic changes produced by the increase in haematocrit. In Kenyan patients with normal or low blood pressure there have been isolated reports of hypertensive crisis with encephalopathy-like symptoms, including headache and confusion, and generalised seizures. Other adverse effects include thrombosis at vascular access sites and clotting in the dialyser, transient increases in the platelet count, flu-like symptoms including chills and myalgia, hyperkalaemia, and skin rashes. There have been rare reports of anaphylactoid reactions. Pure red cell aplasia has been reported rarely in patients with chronic renal failure.
Precautions of Erythropietin in Kenya
Can Erythropoietin/Recormon/Epofit/Relipoietin be Abused in Kenya?
Comments have been published on the dangers of the abuse of recombinant human erythropoietin by athletes as an alternative to “blood doping”
- 1. Scott WC. The abuse of erythropoietin to enhance athletic performance. JAMA 1990; 264: 1660. PubMed
- 2. Adamson JW, Vapnek D. Recombinant erythropoietin to improve athletic performance. N Engl J Med 1991; 324: 698?9. PubMed
- 3. Kennedy MC. Newer drugs used to enhance sporting performance. Med J Aust 2000; 173: 314?17. PubMed
Haematocrit may continue to rise for several days after administration of recombinant human erythropoietin, possibly reaching dangerously high levels. Lack of medical supervision and fluid loss during endurance events increase the risk of serious adverse consequences of changes in blood viscosity produced by such misuse.
Benefits of Recombinant human erythropoietin in Surgery in Kenya.
Concern over the safety of blood transfusions and the need to conserve blood supplies in Kenya has led to interest in methods of reducing blood use in surgery. Recombinant human erythropoietin has been used to increase the number of units harvested for autologous transfusion and to reduce transfusion requirements. It has also been used as an alternative to blood transfusions, with positive results witnessed.
Single-ingredient Preparations of Recombinant human erythropoietin available in Kenya
The symbol ? denotes a preparation which is discontinued or no longer actively marketed.
Kenya; RECORMON, EPOFIT, RELIPOETIN Arg.: Eprex; Hemax; Pronivel; Recormon; Austral.: Eprex; Austria: Culat; Erypo; NeoRecormon; Recormon; Belg.: Eprex; NeoRecormon; Recormon?; Braz.: Eprex; Eritina; Eritromax; Hemax-Eritron; Mepotin; Recormon; Tinax; Canad.: Eprex; Chile: Eprex; Hypercrit; Recormon; Denm.: Eprex; NeoRecormon; Recormon?; Fin.: Eprex; NeoRecormon; Fr.: Eprex; NeoRecormon; Recormon?; Ger.: Eprex; Erypo; NeoRecormon; Recormon?; Gr.: Eprex; NeoRecormon; Hong Kong: Eprex; Recormon; Hung.: Eprex; NeoRecormon; India: Wepox; Irl.: Eprex; NeoRecormon; Recormon?; Israel: Eprex; Recormon; Ital.: Epoxitin; Eprex; Eritrogen?; Globuren; NeoRecormon; Jpn: Epogin; Espo; Malaysia: Eprex; Mex.: Bioyetin; Epomax; Eprex; Exetin-A; Hypercrit; Recormon; Neth.: Eprex; Recormon?; Norw.: Eprex; NeoRecormon; Recormon?; NZ: Eprex; Recormon; Port.: NeoRecormon; Recormon; S.Afr.: Eprex; Recormon; Repotin; Singapore: Eprex; Recormon; Spain: Epopen; Eprex; Erantin?; NeoRecormon; Swed.: Eprex; NeoRecormon; Switz.: Eprex; Recormon; Thai.: Eprex; Hemax; Recormon; UAE: Epotin; UK: Eprex; NeoRecormon; Recormon?; USA: Epogen; Procrit;





Reviews
There are no reviews yet.